The Journey of Life Sciences

Currently, the average life expectancy in the United States is 77.3 years. Medical advancements have evolved to allow humans to reach that age, but it wasn’t always that way.
The humanity of centuries, and even decades ago, dealt with much shorter lifespans and many more challenges in health and medicine. For that reason, we thought we would shed some light on where our modern medical therapies and treatments came from.
Join us as we take you all the way back to the turn of the century and travel up to the modern-day on the Journey of Life Sciences.
Today’s Medical Advancements Progressed Rapidly to This Point
Did you ever think you’d be reading this on a phone the size of a paperweight?
Since the turn of the 20th century, society has progressed rapidly. People were still traveling by horse and buggy in 1900, and now people fly in planes and drive cars that are 100% electric.
The same is true for the history of life science. The technology we use to treat sickness and disease today is nowhere near what we had over 100 years ago. In the late 19th to early 20th century, people were still dying from illnesses like pneumonia in large numbers.
Today, life science development has advanced so far that it’s hard to fathom not having treatment for such a common ailment not so long ago. That’s why we owe it to the men and women responsible to take a look at the path that got us here.
Medical Advancements in the 1900s-1920s
The first two decades of the 20th century set the stage for what life science is as we know it today. New medical testing technologies and global health challenges would begin to change the face of medicine for the next century to come:
1909: Paul Ehrlich develops the first pharmaceutical treatment
In his quest to cure “sleeping sickness,” Ehrlich accidentally accidentally cured syphilis, a sexually transmitted disease that could be very disabling, even fatal, if contracted. Ehrlich’s work started as a way to find a drug designed to kill a germ that enters the body.
Given the nature of syphilis, it wasn’t talked about much but affected countless lives during this period. In just three weeks, Ehrlich and his partner, Sahachiro Hata, worked on his initial findings and quickly developed a complete cure for syphilis. By 1910, the medication was released to the public and sold worldwide under the name Salvarsan.
1914: The electrocardiogram (ECG or EKG) was brought to the U.S. by Dr. Paul Dudley White
This was just one of the many contributions Dr. White made to the area of heart health. He’s credited with founding the American Heart Association (AHA) and being one of the first public advocates of a healthy lifestyle containing physical activity and exercise. Some health experts of the time believed his most significant contribution to the field of life sciences was his passion for “…clinical observation and research at a time when American cardiology was in its infancy.”
1918: The widespread flu pandemic hits
This pandemic started mildly in Spain but turned fatal in just a few months. This worldwide “Spanish Flu” outbreak illuminated the limitations of medicine at the time, shed light on the side effects of war (we were just exiting World War I), and laid the groundwork for how pandemics would be handled in the future. It’s also proof that medicine, much like history, tends to repeat itself.
Doctors of the time tried every known remedy to control the spread of the flu. Therapies like quinine tablets, bleeding, castor oils, baths, and tonics were used to no effect. Eventually, they realized the best way to keep people safe was to prevent the spread through geographic barriers.
A “lockdown” was instituted as local governments began to shut down theaters, churches, and other public places. Cities like New York put emergency ordinances in place making it illegal to spit, cough, or sneeze. City officials threatened fines of up to $500 for violation of these ordinances and people began to wear gauze masks soaked in camphor or another medicine when they left their homes.
We see some similarities to how we handled the COVID-19 pandemic, except at this point we already knew how viral infections spread, and we were able to implement lockdowns and masks much faster.
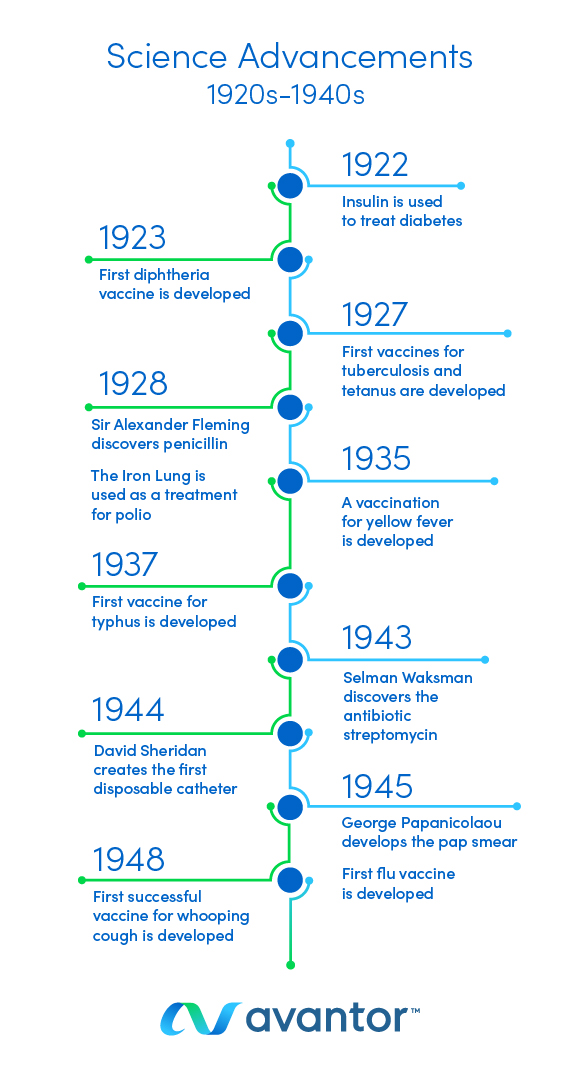
Medical Advancements in the 1920s-1940s
Fast forward to the mid-to-late 1920s to 1940s. The “Gatsby Era.” The time of flappers, prohibition, and mint juleps.
The world had just been rocked by the flu pandemic of 1918. The medical community was made aware of exactly how much it didn’t know, in a big way. But the flu pandemic would be a learning experience that would shape the history of life science. We begin to see worldwide breakthroughs in the treatment of illnesses and vaccines, including the first vaccinations for the flu itself:
1922: Insulin is used to treat diabetes
Diabetes was a disease previously regarded as incurable and untreatable. In 1922, scientists had already made the connection between the pancreas and diabetes. They even isolated the “sugar disease” to a small section of the pancreas known as the Islets of Langerhans.
A scientist named Frederick Banting, and his assistant, Charles Best, isolated the hormones from the Islets of Langerhans, which they later called “insulin,” and administered it to 10 diabetic dogs. The treatment was a success. It was then refined and purified and finally ready for human use later that year when it was used to successfully treat a 14-year old boy who was dying of diabetes. Banting and Best went on to win a Nobel Prize for their work in 1923.
1923: The first diphtheria vaccine is developed
In 1921, there were 206,000 diphtheria cases in the U.S. Death rates for diphtheria were around 20% for people under age 5 and over age 40 and 5-10% in people between the ages of 5 and 40. Thanks to the creation of the vaccine, no recent cases of diphtheria have been reported in America. However, this disease still affects the global population.
1927: The first vaccines for tuberculosis and tetanus are developed
French scientists Albert Calmette and Camille Guérin discovered the vaccine from a weakened form of the tuberculosis bacteria (known as BCG) in cows. Dr. Benjamin Weill-Hall, a French pediatrician, was the first to administer the vaccine to a child. The tetanus vaccine was developed in 1927 but didn’t see widespread adoption until the start of World War II (1938), when a more effective absorbed version of the vaccine was developed. This new version of the vaccine reduced tetanus infection rates in soldiers by 95%.
1928: Sir Alexander Fleming discovers penicillin
Fleming knew how deadly infectious bacteria could be from his time in World War I. He began growing bacteria in Petri dishes to work on formulating a treatment but discovered penicillin purely by accident when he noticed mold growing in one of his samples.
In a fit of absent-mindedness, Fleming left his Petri dishes unattended for some time, allowing mold spores to grow in his bacteria samples. Most of the samples were ruined, but when Fleming examined a few of them under a microscope, he noticed the mold effectively fighting off some strains of bacteria. Subsequent lab work would lead to the discovery that penicillin was the substance responsible for fighting off the bacteria.
Fleming’s made his discovery in 1928, but widespread penicillin production didn’t happen until 1943. That was just in time to meet the antibacterial needs of yet another global war effort, World War II.
1928: The Iron Lung is used as a treatment for polio
The same year penicillin was discovered, doctors noticed that people in the early stages of polio had trouble breathing as the disease paralyzed the muscles in their chest. Nothing seemed to work until Philip Drinker and Louis Agassiz Shaw invented the tank respirator (aka Iron Lung), which facilitated respiration in polio patients until they recovered enough to breathe independently. Eventually, John Emerson would improve their design, making the Iron Lung more affordable and ready for general use. Until then, there were rooms filled with Iron Lungs for patients to use and improve their condition.
1935: A vaccination for yellow fever is developed
Max Theiler and his colleagues are responsible for creating the yellow fever vaccine. They did so by passing the initial vaccine through tissue from chicken egg embryos and mice. Passing the virus through this tissue eventually lead to an attenuated version of the vaccine safe for use in primates and humans.
Unlike other vaccines up until this point, this vaccine was quickly adopted and prepared for mass consumption. Theiler discovered a safe, distributable version of the vaccine in 1937 and by the time the U.S. entered World War II in 1941, just 4 years later, 4 million doses of the vaccine had been distributed worldwide.
1937: The first vaccine for typhus is developed
Typhus is a bacterial disease that originated during the 15th century. By the 19th century, the infectious bacteria already had a pandemic reputation, claiming hundreds of thousands of lives during the War of 1812.
In 1937, as another war was fast approaching, Polish scientist Rudolf Weigl developed a technique to infect experimental lice with the typhus virus. These lice then became the incubator for what would become the typhus vaccine. Weigl’s work would go on to play a very interesting role in Nazi-occupied Poland and the early stages of World War II.
1943: Selman Waksman discovers the antibiotic streptomycin
Unlike the work of Alexander Fleming, Waksman’s discovery of streptomycin was not accidental. It was the result of hard work and testing thousands of microbe samples.
Eventually, in 1943, Waksman and his graduate students isolated the antibiotic streptomycin. The discovery was significant because streptomycin was effective against gram-negative bacteria, an area where penicillin fell short. Streptomycin also proved to be effective against in-vitro cases of tuberculosis, also known as The Great White Plague, and is still in use today.
1944: David Sheridan creates the first disposable catheter
Catheters are used to help some patients drain waste and receive medication and nutrients. In 1944, however, these devices were somewhat primitive and ineffective.
Sheridan, an inventor, decided to try his hand in the catheter business and created the hollow, plastic tube that would inspire modern versions of the device. His improvements also saved thousands of lives by drastically reducing the risk of infection, because his were disposable and not reused.
1945: The first flu vaccine is developed
Scientists and doctors worldwide were still searching for a cure for the flu after the outbreak of 1918. The first influenza vaccine shows the cyclical, repetitive nature of the history of life science.
Scientists looked at research conducted years earlier by Louis Pasteur and saw he could develop a rabies vaccine by using a strain of the rabies virus. This same method was used to create the first flu vaccine.
Researchers altered and tested the vaccine until trial patients only showed mild influenza symptoms. Then, it was approved for mass adoption and distributed to address the growing flu concerns among factory workers.
1945: George Papanicolaou develops the pap smear
The same year as the flu vaccine, George Papanicolaou started saving countless lives by pioneering the advancement of women’s health with his invention, the Pap smear test. His work became instrumental in diagnosing cervical cancer in its early stages.
In 2021, 14,480 new cases of cervical cancer and 4,290 deaths occurred in the U.S. Without the work of George Papanicolau, those numbers could be much higher as Pap smears are screening tests that are used yearly to help screen women for cervical cancer.
1948: The first successful vaccine for whooping cough is developed
The first vaccine had been attempted as early as 1914, without much success. After a large outbreak, Leila Denmark, a pediatrician, investigated this disease for six years. At a similar time in the 1940s, two other women, Pearl Kendrick and Grace Eldering, developed the vaccine known as DTP, which was widely considered the successful version of the vaccine. It was replaced by safer, acellular forms of the vaccine with lower chances of harmful side effects.
Vaccines for diptheria, tetanus, and pertussis (whooping cough) were eventually blended into one treatment known as the DTP vaccine. But this medication still relied on whole cells of the viruses to be effective. Using full-strength forms of the virus for treatment resulted in a high rate of harmful side effects in vaccinated patients.
Eventually the DTaP vaccine, an acellular weakened form of the original, was licensed and became available for commercial use. Since this newer vaccine relied on an attenuated or weakened strain of the viruses, side effects were lower, and the medication was safer for use.
Throughout the 20th century, America experienced approximately 200,000 cases of whooping cough per year. In 2020, that number was down to just 5,000 cases nationwide.
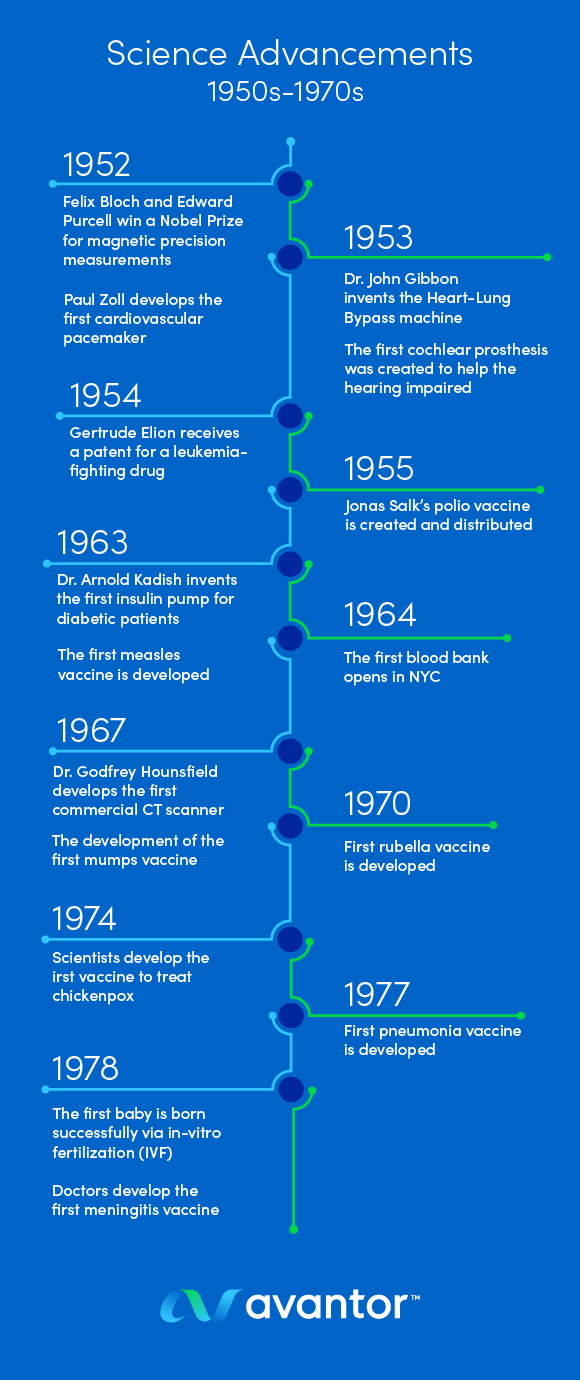
Medical Advancements in the 1950s-1970s
From the 1950s to the 1970s, modern life science development began to take shape. Doctors began to expand on the treatments that were pioneered in the previous era, as well as study medicine on a deeper level:
1952: Felix Bloch and Edward Purcell win a Nobel Prize for magnetic precision measurements
Bloch and Purcell’s discoveries would be the foundation for MRI technology. Their Nobel Prize was awarded in the area known as Magnetic Resonance. Essentially, this technology could display the detailed structure of a molecule. This is the technology that MRIs, or Magnetic Resonance Images, are founded on. However, the first official MRI exam wouldn’t take place until almost 30 years later, in 1977.
While this was the impetus for amazing strides in the fields of chemical and physical analysis, it presented some challenges with commercial use in human patients.
Other scientists like Raymond Damadian, Paul Lauterbur, and Peter Mansfield were all instrumental in evolving NMR technology for commercial use. Bloch and Purcell’s initial discovery needed to be refined into a technology known as a gradient magnetic field. This allowed 2-dimensional images to be layered in a way that creates a 3D view. This was the missing link that allowed Damadian to finally conduct the first full-body MRI scan in 1977.
1952: Paul Zoll develops the first cardiovascular pacemaker
This is part of a more significant trend of medical engineering we begin to see throughout these 20 years of life science development. The major innovation here is that Zoll developed a pacemaker that could be surgically implanted and left to run automatically.
A previous version of the pacemaker had been made in the 1930s, but this version needed to be hand-cranked by a physician. This initial pacemaker was developed by Albert Hyman and his brother, who was an engineer. It required a needle being inserted through the patient’s chest wall.
This needle was attached to a spring motor and hand crank that worked to generate the electricity necessary to stimulate heart function. While this technology was revolutionary for the time, it didn’t make living life with heart problems any easier. Zoll’s work, on the other hand, has undoubtedly made life easier for millions of people worldwide with his work.
1953: Dr. John Gibbon invents the Heart-Lung Bypass machine
In 1953, Gibbon’s device was also successfully used during surgery for the first time. With heart problems being what they are worldwide, open bypass surgery has become a much more popular procedure in recent decades. This life-saving surgery wouldn’t be possible without Gibbon’s invention. His machine is vital to keeping the heart and lungs working during the bypass procedure. With heart disease being one of the leading causes of death, this bypass machine has helped to save countless lives over the years.
1953: The first cochlear prosthesis was created to help the hearing impaired
The technology was pioneered by Andre Djourno, a French researcher and med school professor. During an experiment, Djourno discovered that deaf participants could hear background noise if certain auditory nerves were stimulated with electric impulses. This discovery led to the creation of the first cochlear prosthesis which was later adapted for the first implantation procedure.
Research on cochlear implants hit its stride during the 1960s, when multiple implantations were done and doctors discovered the importance of the placement of the electrodes. From the 1970s through the 1990s, a multi-channel cochlear device was invented, allowing the deaf to experience multiple levels of sound. Shortly thereafter, cochlear technology was given its stamp of approval by the FDA in 1984 as an official medical treatment for hearing impairment.
1954: Gertrude Elion receives a patent for a leukemia-fighting drug
Gertrude Elion, a biochemist, discovered a pharmaceutical treatment for leukemia through her work with purine compounds. Purines are the basis for DNA, and Elion found that certain compounds could prevent DNA replication. By manipulating various purine compounds, Elion created a drug that works to fight cancer the same way as chemotherapy treatment. Her work earned her a Nobel Prize and would go on to cure 80% of children who had leukemia.
1955: Jonas Salk’s polio vaccine is created and distributed
Not only did this vaccine treat polio, but it made great advancements for the development of vaccines in general. By August 1955, 4 million people had received . His work took the number of polio cases down from 28,985 in 1955 to 5,894 just two years later, in 1957.
Researchers were also prompted to pioneer cutting-edge vaccination procedures during their work with polio. These revolutionary changes in medical engineering would become the foundation for the widespread production of vaccinations to fight illnesses like measles, mumps, and smallpox.
1963: Dr. Arnold Kadish invents the first insulin pump for diabetic patients
Before Kadish’s work on the insulin pump, diabetes patients needed to coordinate several insulin injections per day to regulate their blood glucose levels. The insulin pump made these injections obsolete, and monitoring blood glucose levels became more manageable.
Kadish’s insulin pump would be the inspiration for the wearable pump that would come a decade later, in 1973. The pump he made in 1963 was technically wearable, but it was essentially a synthetic pancreas worn on the back as a cumbersome backpack. The device effectively delivered insulin and glucagon to the wearer but wasn’t portable enough to be an “everyday” device.
1963: The first measles vaccine is developed
Biomedical scientist John Enders is responsible for the initial measles vaccine. This first version of the vaccine was adequate, but it wasn’t the version of the measles vaccine we know today. That vaccine was created five years later in 1968. The second version of the vaccine was weaker than Enders’ vaccine and ready for distribution. Since 1968, this second version of the vaccine has been the only version used in the United States and played a crucial role in 85% of the global population receiving the measles vaccine by 2013. However, over time, changes were made to it, including a second dose of the MMR vaccine for children following an outbreak in 1989. In 2000, measles was declared eliminated in the United States. Despite the great success, due to international travelers and anti-vaccine sentiment, measles has reemerged in small numbers.
1964: The first blood bank opens in NYC
This signifies the first successful large-scale, long-term blood storage effort by scientists. Dr. Aaron Kellner was appointed the first president of the New York Blood Center (NYBC) and is credited with the large-scale collection and storage of blood, as well as launching research programs on how blood relates to illnesses like heart disease. Today, the NYBC has evolved to the point of collecting over 4,000 blood samples per day and, with the help of its partners, impacts more than 75 million American lives.
1967: The development of the first mumps vaccine
The mumps vaccine is known throughout the medical community as one of the fastest vaccines to go to market. It all started when a researcher at Merck, the pharmaceutical giant of the time, swabbed his daughter’s throat to create a weakened version of the vaccine.
It only took four years to create a distributable version of the mumps vaccine from that moment. This speed is thanks, in large part, to the earlier vaccine research done in the 1940s and 50s for polio and measles.
1967: Dr. Godfrey Hounsfield develops the first CT scanner for commercial use
Hounsfield’s work didn’t take long to make an impact. In 1971, his CT scan was used during its first surgical procedure in London, England, where his prototype was used to scan a patient diagnosed with a frontal lobe brain tumor.
Images from Hounsfield’s CT, or computed tomography, scan confirmed the diagnosis, and a surgeon operated on the tumor shortly after that. The surgeon who performed the procedure commented that the actual tumor looked “just like the [CT scan] image.”
Hounsfield’s prototype produced grainy, 80 x 80 matrix images, and each scan took about 5 minutes to complete. Today, thanks to Hounsfield’s work, the technology has evolved to produce high-resolution images in an average of approximately 0.3 seconds.
1970: The first rubella vaccine is developed
The development of the rubella vaccine came in the wake of a rubella pandemic that spanned the entire U.S. in 1964-65. During this time, 12.5 million cases of rubella were reported.
Famed researcher Maurice Hilleman is responsible for developing the first vaccine. A year later, in 1971, a combination Measles-Mumps-Rubella (MMR) vaccine was licensed. This combination vaccine was used until rubella was officially eliminated in from the United States in 2004.
1974: Scientists develop the first vaccine to treat chickenpox
Japanese scientist, Michiaki Takahashi, developed the Oka strain of the chickenpox virus. This live, attenuated strain of chickenpox became the basis for the first vaccine.
Eventually, Maurice Hilleman and his colleagues at Merck would refine Takahashi’s discovery into a distributable vaccine version in 1984. The vaccine became part of the standard pediatric vaccination schedule in 1995 and is currently on the World Health Organization’s Model List of Essential Medicines.
1977: The first pneumonia vaccine is developed
A few years after the chickenpox vaccine, the first licensed pneumonia vaccine was produced, but this vaccine was built on work that started decades earlier. Doctors and scientists had been fighting pneumonia since the turn of the 20th century, all the way up through World War II combat. In the early stages, however, pneumonia was primarily treated by antibiotics.
This presented a challenge, as most strains of pneumonia began to develop immunity to antibiotic treatment. The 1977 vaccine solved this issue and was approved for widespread distribution to certain patients 2 years and older in 1978, just one year later. Over the years, the vaccine has been tweaked and updated, building off of the science behind it in 1977 to be the vaccine we know today.
1978: The first baby is successfully born via in-vitro fertilization (IVF)
Louise Joy Brown, the world’s first “test-tube baby,” was born on July 25, 1978. The procedure was done in Manchester, England, and Louise was a healthy baby delivered by C-section, weighing in at 5 pounds, 12 ounces. The Browns would go on to have a second child, Natalie, via IVF. Natalie became the first IVF-born child to have a child of her own in May 1999 by natural birth.
1978: Doctors develop the first meningitis vaccine
While 1978 was the first year the meningitis vaccine was distributed for widespread use, meningitis vaccine research began much earlier. Researchers were looking into cures for the disease as early as the 1960s, and a vaccine had been created and approved for U.S. service members as early as 1971.
In 1975, improvements were made to that original version of the vaccine and even more improvements were made by 1978. This final vaccine version treated the two most devastating forms of the disease, meningitis serogroup A and C.
Medical Advancements in the 1980s-2010s
Now, we begin to enter the “modern age” in our history of life science. Coming into the 1980s, the world began to see other significant advancements in the world of vaccines, including the complete eradication of a major disease.
During this period, we also start to see the early stages of treatments for major diseases like AIDS and cancer, as well as the beginning of our work with DNA and the human genome:
1980: Smallpox is officially declared eradicated thanks to the advancements in vaccines
This may be one of the biggest wins for life science development on this timeline. Smallpox devastated humankind for almost 3,000 years, and the vaccine was actually created in 1796, nearly 200 years prior to eradicating the disease. In fact, the disease may have never been eradicated if the World Health Organization (WHO) hadn’t championed a concerted effort to wipe it out beginning in 1967.
The WHO initiated a worldwide vaccination and monitoring plan until the last natural case was reported 10 years later, in 1977, in Somalia. Three short years after that, in 1980, smallpox was officially declared eradicated.
1981: The first vaccine was developed for hepatitis B
Microbiologist Irving Millman developed a blood test to screen for the hepatitis B virus in 1971. Blood donations could be screened for the virus and, as a result, hepatitis B infections by transfusion decreased by 25%.
This blood test also became important for the vaccine. The vaccine was an “inactive” vaccine created by blood donations infected with the virus. It was approved by the FDA in 1981 and distributed by Merck, a pharmaceutical company. However, this version of the hepatitis B vaccine, known as Heptamax, was discontinued in 1990.
1983: HIV is identified by scientists as the cause of AIDS
Scientists in the Pasteur Institute of France isolated HIV as the cause of the disease, and a blood test was created to screen for the virus. Scientists hoped to have a vaccination to combat HIV within two years of this discovery.
Unfortunately, things didn’t go as planned, and more than 400,000 AIDS deaths occurred from 1980 to 1990. Progress was made soon after in 1995 when the FDA approved the first protease inhibitor. This medical advancement began a new age for antiretroviral treatment and dropped the AIDS mortality rate by 80%.
1992: Researchers develop the first vaccine for hepatitis A
Maurice Hilleman and his team at Merck are responsible for bringing this vaccine and many others to market. The treatment became known as Vaqta, and although it was created in 1992, it wouldn’t be licensed until 1995.
Vaqta has been instrumental in prolonging human life, as the vaccine can last from 20 years to a person’s entire lifespan. Historically, Vaqta has effectively .
1996: Scientists completed the first successful cloning of a sheep named Dolly
Scientists took a mammary gland from adult Finn Dorset ewe and stimulated it with electrical impulses to begin the cloning process. Eventually, the mammary gland cell nucleus fused with a host egg and began to divide.
Dolly was a complete genetic copy of the Finn Dorset ewe and lived a long, healthy life. The technology used to clone her is now called Somatic Cell Nuclear Transfer (SCNT) and has been used to clone a variety of complex mammals, including primates, successfully.
2000s: Stem Cell Research
Doctors begin using advancements in stem cell research as medical treatment. During this time, stem cells are used worldwide to treat diseases like cancer, save unborn children, repair limbs, and more. The extraction of stem cells was discovered 20 years earlier, during the 1980s. Scientists then began to hit their stride, studying stem cells on a much deeper level, in the late 1990s. Pioneering their use as a viable medical treatment would come about in the early 2000s.
In 2006, scientists discovered they could “reprogram” specific specialized adult cells and return them to a “stem cell-like” state. In the medical community, these are now known as induced pluripotent stem cells (iPSCs), and they have significant implications for curing degenerative diseases and much more.
2003: A worldwide collaboration of scientists complete the Human Genome Project and successfully map the entire genetic blueprint of human DNA
The completion of the Human Genome Project represented a culmination of almost 15 years of work by thousands of scientists worldwide. There are parts of the human genome that are still too complex to map, but scientists say it’s likely that those areas don’t contain many gene sequences.
The final sequence, approved by an international group of scientists, covers 99% of the human genome and is 99.99% accurate. This complete picture of human genetic makeup bodes well for the early diagnosis and prevention of disease, the widespread availability of gene mapping, and the development of new medications.
2006: The HPV vaccine is created
This is the first vaccine created to target a cause of cancer. Merck & Company produced the vaccine Gardasil to protect against significant strains of HPV.
The vaccine protects against nine strains of the virus, including the four most associated with cervical cancer. High-risk HPV strains cause over 90% of cervical cancer cases, but that number continues to fall by 1.6% year after year.
While much has been done to reduce instances of cervical cancer in the U.S., it’s still a concern as scientists predict 14,100 new cervical cancer cases in 2022. Researchers will continue to expand on the amazing work they’ve already done in the fight against cervical cancer and reduce the number of cases.
2008: mRNA vaccines are used to treat cancer
The science community experiences advancements in vaccine and cancer research as 13 melanoma patients are treated with an mRNA vaccine as early as 2008. The technique uses a portion of the cancer’s mRNA or genetic code to provoke an immune system response in patients.
This innovative treatment was successful in reducing lesions associated with cancer, as well as fighting solid tumors. In fact, it was so successful in fighting a tricky disease like cancer that we will see this advancement in vaccine technology used again, over a decade later.
Medical Advancements Through 2021
As society moved into the 21st century, we began to see modern advancements in medicine involving DNA and stem cells. The interesting thing, however, is that we also see advancements in vaccines and global pandemics that built on medical treatments started almost 100 years ago, early on in the history of life science:
2020/2021: mRNA vaccine technology is used to create a vaccine against COVID-19
The COVID-19 vaccine saved countless lives and prevented severe illness by building on the mRNA technology used to treat melanoma back in 2008. mRNA vaccine technology works by introducing a piece of the virus’ mRNA to the body and allowing the immune system to produce antibodies without exposing the patient to the virus itself.
The antibodies produced by the mRNA treatment also stay in the body longer and react much more quickly to future infections. This was key to controlling the spread of a pandemic virus with high transmission rates like COVID-19. As we learned from the flu pandemic back in 1918, controlling viral infections like this requires several steps from isolating and avoiding those who are sick, as well as having vaccines to help bolster immune systems.
The Journey of Life Sciences Never Ends
Throughout the past 100-plus years, we’ve seen the history of life science grow by incredible leaps and bounds. But the common thread is that the journey is a ladder, constantly building on advancements made in the past to treat the medical challenges of the future. Without the beginning rungs of the ladder, science would have been unable to move forward.
We hope this journey through time has given you more insight into where we came from, where we are, and where we’re going in the development of life science. Where we’ve grown to, as a society, is truly amazing, and we’re excited to see what the future has in store for science and medicine.